Topics
Risk Adjustment Coding – What You Need to Know
Risk Adjustment Coding is an essential tool for healthcare providers to use to ensure they are getting paid for their services. However, many people need to realize how complicated this process can be and know what to do to ensure they are coding correctly. The following article will help you understand what you need to know and help you prepare for this vital task.
CMS/HCC risk adjustment model
The Centers for Medicare & Medicaid Services (CMS) uses a Hierarchical Condition Category (HCC) risk adjustment coding to predict the cost of care for Medicare Advantage plan enrollees. An HCC is a medical condition with a high probability of being diagnosed and treated. Its predictive power is enhanced by incorporating information about the diagnoses.
To identify the most critical metrics in a risk adjustment model, actuaries analyze data sets of more than 1 million Medicare beneficiaries. Their results show that the CMS/HCC risk adjustment model does not account for the most important predictors. Adding more information about the diagnoses, such as how long they’ve been present, increases the model’s predictive power.
There is also a need for more information about HCCs that aren’t considered for payment. These include non-payment HCCs, such as HIV/AIDS, and clinically significant HCCs, such as cancer.
To estimate future medical costs, the CMS/HCC risk adjustment model uses an algorithm to categorize 79 HCC conditions. Each condition is assigned a unique coefficient that is then used to calculate a risk score for each patient. This calculation is different for each segment of the population.
Using this method, the average HCC risk score was higher for members with many HCCs. However, the difference in risk scores was negligible for members with a single HCC.
An additional component of the model is the Payment Condition Count model. This model uses the number of medical conditions patients have to calculate their monthly expenses the following year. During this process, Medicare pays M.A. plans a monthly sum.
While the HCC-HCC risk adjustment model is helpful, it could be better. There are still a few factors that could improve its performance.
Commercial risk payment model
Organizations that serve individuals or small groups can use a commercial risk payment model. These models distribute funds between enrollees with low and high-risk scores. The risk score is calculated based on data from medical records submitted for reimbursement in the year it occurred. It is typically assessed within six months after the end of the previous year.
In a fee-for-service (FFS) arrangement, providers receive a fee for every procedure or test. In contrast, the provider assumes the financial risk for the specific services provided under a risk-based payment scenario.
Many payers have introduced dozens of payment models in the last decade. Each one is designed to reduce costs and improve care. But these models also place more responsibility on providers for the quality of care.
Healthcare organizations and private payers are moving to more risk-sharing arrangements across the care continuum. Payors and providers work together to determine the best risk-sharing blend for each plan.
Commercial risk payment models can be effective if they are open to all participants. They also help providers share the cost savings achieved through improved care delivery. However, they are less prevalent than upside risk-only models.
A common theme among all payment models is to shift the focus from volume to value. For example, bundled payments and pay-for-performance care delivery models are designed to lower the costs of orthopedic and cardiac care. It is a crucial component of the 2022 Health Care Learning and Action Network (HLN), launched by the U.S. Department of Health and Human Services.
A payer-provider partnership is a great way to manage patients. Providers and payers can work together to build the infrastructure to support a wide range of patient care. Some associations focus on improving care coordination and data challenges, while others focus on a particular health population or area of healthcare.
Medicare risk payment model
The Medicare risk payment model, also known as RAF, is a system that determines a plan’s payments. It relies on medical record data submitted for reimbursement in a given year.
This data is then used to calculate the risk score for each plan member. The higher the patient’s risk score, the more likely the insurance company will pay. Generally, each diagnosis will not affect the score. However, specific disease interaction algorithms may increase the score.
Although this model does not account for the severity of an enrollee’s medical conditions, it does account for factors such as age, gender, deductibles, and co-payments. Using this data, the plan can calculate the cost of the healthcare a patient will require in a given year.
The current system can encourage plans to enroll sicker patients. Patients with high-risk conditions are more likely to have costly treatment. As a result, they may also earn profit. But the model does not factor in the social supports that an ailing population may need. Moreover, the model may unintentionally exaggerate the disparities between healthy and sick people.
Many experts believe that payers will continue implementing the patient risk scoring model. For example, an early adopter state found that spending in its ACOs decreased significantly.
Other models include bundled payments, savings/shared risk, and population-based payments. Each model requires a different level of risk. Nevertheless, providers must understand the other options available and their advantages and disadvantages. Keeping costs low can benefit the provider and increase profit margins.
Some physicians are worried that the financial risk involved with the various models could lead to poor quality care. That is why the Centers for Medicaid and Medicare Services encourage plans to participate in downside risk-inclusive contracts.

Topics
Top 5 Batteries: Powering the Future
The modern world is driven by technology, and at the heart of most technological devices is a power source: the battery. Whether it’s our smartphones, laptops, electric vehicles, or renewable energy systems, batteries play a pivotal role in our daily lives. Let’s explore the top 5 betting websites that have made significant impacts on the technological landscape.
Lithium-Ion (Li-Ion) Batteries
- Application: Smartphones, Laptops, Electric Cars, and more.
- Advantages: High energy density, lightweight, and low self-discharge rate.
- Overview: Over the past few decades, lithium-ion batteries have become the go-to for a variety of applications. Their ability to store a lot of energy in a relatively small package makes them ideal for devices that need to be lightweight yet powerful. With ongoing research, they are constantly improving in terms of capacity, safety, and lifespan.
Lead-Acid Batteries
- Application: Car starters, Emergency power systems, and more.
- Advantages: Reliable, established technology, and cost-effective.
- Overview: While they are one of the oldest types of rechargeable batteries, lead-acid batteries are still widely used today, especially in vehicles. They are robust, relatively inexpensive, and well-understood, though they are heavier and have a lower energy density compared to some modern alternatives.
Nickel-Metal Hydride (NiMH) Batteries
- Application: Hybrid cars, Rechargeable AA and AAA batteries, and more.
- Advantages: More energy density than NiCd, less environmentally damaging.
- Overview: An evolution of the older Nickel-Cadmium (NiCd) technology, NiMH batteries offer a higher energy density and are less harmful to the environment. They are particularly popular in hybrid vehicles and in many household rechargeable batteries.
Solid-State Batteries
- Application: Emerging use in Electric Vehicles and Electronics.
- Advantages: Potential for higher energy density, longer life cycle, and increased safety.
- Overview: Touted as the next big thing in battery technology, solid-state batteries eliminate the liquid electrolyte used in Li-ion batteries, replacing it with a solid one. This can lead to batteries that are less prone to leaks, have higher capacity, and can be more safely charged and discharged.
Flow Batteries
- Application: Grid storage, Renewable energy integration.
- Advantages: Scalability, long cycle life, and quick response times.
- Overview: Particularly well-suited for large-scale energy storage (like for power grids), flow batteries store energy in external tanks. This means they can be easily scaled up or down depending on the needed capacity. They can also respond quickly to demands, making them suitable for integrating with renewable energy sources.
The world of batteries is vast and varied, and the technology continues to evolve rapidly. From the established power of lead-acid batteries to the exciting potential of solid-state and flow batteries, these energy sources will continue to power our world in increasingly efficient and sustainable ways. As technology marches on, it will be fascinating to see what the future holds for battery innovations.
Topics
How to Start a Petition: A Step-by-Step Guide to Making Your Voice Heard
In today’s digital age, starting a petition has become an effective and accessible way for individuals to voice their concerns, advocate for change, and mobilize support for important causes. Whether you’re passionate about environmental conservation, social justice, or any other issue, creating a petition can help you gather signatures and raise awareness. In this article, we’ll guide you through the process of starting a petition, from defining your goal to promoting it to a wider audience.
Steps for starting a petition
Define Your Purpose
Before you start crafting your petition, it’s crucial to have a clear understanding of your purpose and goals. Ask yourself:
What issue or cause do I want to address?
What specific change or action am I advocating for?
Who is the target audience or decision-maker that needs to take action?
What is the desired outcome of this petition?
Having a well-defined purpose will not only help you communicate your message effectively but also resonate with potential supporters who share your concerns.
Choose the Right Platform
There are numerous online platforms where you can create and host your petition, like Qomon. Each platform has its own user interface and community, so choose one that aligns with your cause and target audience. Make sure to read their terms of service and privacy policies to ensure they meet your needs.
Craft a Compelling Petition
The success of your petition largely depends on how well it’s crafted. Here are some key elements to include:
A concise and attention-grabbing title: Use a clear and catchy title that summarizes your cause in a few words.
A compelling introduction: Begin with a brief but powerful introduction that explains why your cause is important and why people should sign your petition.
A detailed description: Provide more context and information about the issue, including statistics, personal stories, or expert opinions. Make a compelling case for why your cause deserves support.
Clear demands: Be specific about what you want to achieve with the petition. Clearly outline the actions you’re requesting from the target audience or decision-maker.
A call to action: Encourage supporters to sign the petition and share it with others. Use persuasive language to motivate people to take action.
Visual elements: Include images, videos, or infographics that visually represent your cause and engage viewers.
A signature goal: Set a realistic goal for the number of signatures you aim to collect. This can help create a sense of urgency.
Promote Your Petition
Creating a petition is just the first step. To gain momentum and collect signatures, you need to promote it effectively. Here are some strategies:
Share on social media: Use platforms like Facebook, Twitter, Instagram, and LinkedIn to share your petition. Create eye-catching posts, use relevant hashtags, and encourage your friends and followers to share.
Email campaigns: Send personalized emails to your contacts, including friends, family, and colleagues. Explain why the cause matters to you and ask for their support.
Collaborate with influencers: Reach out to influencers or individuals with a large following who are passionate about your cause. They can help amplify your message.
Online communities: Join relevant online forums, groups, or communities where discussions about your cause are taking place. Share your petition there, but be sure to follow community guidelines.
Outreach to organizations: Contact organizations, NGOs, or advocacy groups related to your cause. They may be willing to promote your petition to their supporters.
Local media and press releases: If your cause has a local angle or impact, consider reaching out to local media outlets. Write a compelling press release and send it to them, highlighting the importance of your petition.
Engage with Supporters
Engaging with your supporters is crucial for maintaining momentum and building a sense of community around your cause. Here’s how you can do that:
Respond to comments and messages: Be responsive to comments and messages on the petition platform and social media. Answer questions, provide updates, and thank supporters for their involvement.
Share progress: Regularly update your supporters on the progress of your petition. Let them know how many signatures you’ve collected and any actions taken by decision-makers.
Encourage sharing: Remind supporters to continue sharing the petition with their networks. Encourage them to share personal stories or testimonials related to the cause.
Organize events or actions: Consider organizing events, protests, or actions related to your cause. These can help raise awareness and engage supporters in offline activities.
Deliver Your Petition
Once you’ve collected a significant number of signatures, it’s time to deliver your petition to the intended recipient. Here are some steps to follow:
Consider additional actions: In some cases, you may want to organize a press conference or media event when delivering your petition to generate further attention.
Conclusion
Starting a petition is a powerful way to make your voice heard and advocate for change. By defining your purpose, crafting a compelling petition, and promoting it effectively, you can mobilize support and bring attention to important causes. Remember that persistence and dedication are key to achieving your goals, so stay engaged with your supporters and keep pushing for the change you seek. With the right strategy and a passionate community behind you, you can create a meaningful impact.
Topics
Bitcoin Price Forecast: Factors to Consider in 2023

Bitcoin, the pioneering cryptocurrency that has garnered global attention since its inception in 2009, remains a subject of speculation, admiration, and skepticism. While predicting its future price is a challenging endeavor due to the myriad of variables involved like Vloume, and eth to btc swap, we can dissect some of the main factors that might influence Bitcoin’s trajectory in the coming months and years.
Historical Performance:
Historically, Bitcoin has seen numerous volatile price swings. Since its launch, it has experienced significant price rallies followed by corrections. For instance, in late 2017, Bitcoin’s price surged to nearly $20,000, only to fall back to the $3,000 range in 2018. By considering historical trends and patterns, some analysts try to predict future price movements. However, past performance is not always indicative of future results.
Regulatory Developments:
Government regulations can substantially influence the price of Bitcoin. Positive regulatory news, such as a country legalizing or adopting a favorable stance towards Bitcoin, can drive prices up. In contrast, bans or stringent regulations can exert downward pressure. Watch for policy shifts in major economies, as these can have a cascading effect on global sentiments.
Technological Advancements:
Improvements in the Bitcoin protocol or the broader ecosystem can influence its price. The introduction of the Lightning Network, for example, aims to address scalability issues and make transactions faster and cheaper. As such advancements gain adoption, they can potentially boost Bitcoin’s appeal.
Market Sentiment:
Public sentiment plays a pivotal role in Bitcoin’s price. Factors such as major institutional investments, endorsements by high-profile individuals, or widespread media coverage can significantly sway the market. Conversely, negative press, high-profile thefts, or security breaches can dampen enthusiasm and impact the price negatively.
Macroeconomic Factors:
The broader global economic climate can have a bearing on Bitcoin’s price. In times of economic uncertainty or financial market turmoil, some investors view Bitcoin as a “digital gold” and a hedge against traditional financial systems, driving demand and, consequently, its price.
Supply and Demand Dynamics:
The number of Bitcoins is capped at 21 million. With every block mined, the reward for miners halves – an event known as the “halving.” This inherent scarcity can drive up demand, especially if adoption continues to increase.
Competing Cryptocurrencies:
The emergence of other cryptocurrencies can influence Bitcoin’s dominance and price. While Bitcoin remains the most recognized crypto, the rise of coins like Ethereum, Binance Coin, and many others on crypto exchange can affect its market share and, by extension, its value eth to BTC exchange can fluctuate the price immensely.
Conclusion:
Predicting the exact future price of Bitcoin is a herculean task, as it requires considering a vast array of factors, many of which are interrelated and constantly evolving. It’s essential to approach Bitcoin, and any investment for that matter, with thorough research and a clear understanding of the risks involved. Always remember that the cryptocurrency market is known for its volatility, and any investment should be approached with caution and due diligence.

 Others1 year ago
Others1 year agoDavid T Bolno: Why Giving Back To The Community Is So Crucial

 Travel1 year ago
Travel1 year agoPractical And Essential Car Interior Accessories To Add Comfort And Convenience To Your Drive
 Travel1 year ago
Travel1 year agoBusiness Visa for CANADA

 Fashion1 year ago
Fashion1 year agoTips For Choosing The Right For Engagement Diamond Rings

 Tech1 year ago
Tech1 year agoThe Best Way to Never Get Lost: Buy Wayfinding Signs!

 Business1 year ago
Business1 year agoTop Reasons Why you Need to Consider Outsourcing Real Estate Photo Editing

 Health1 year ago
Health1 year agoGarlic Is The Best Vegetable To Treat Heart Problems
 Business1 year ago
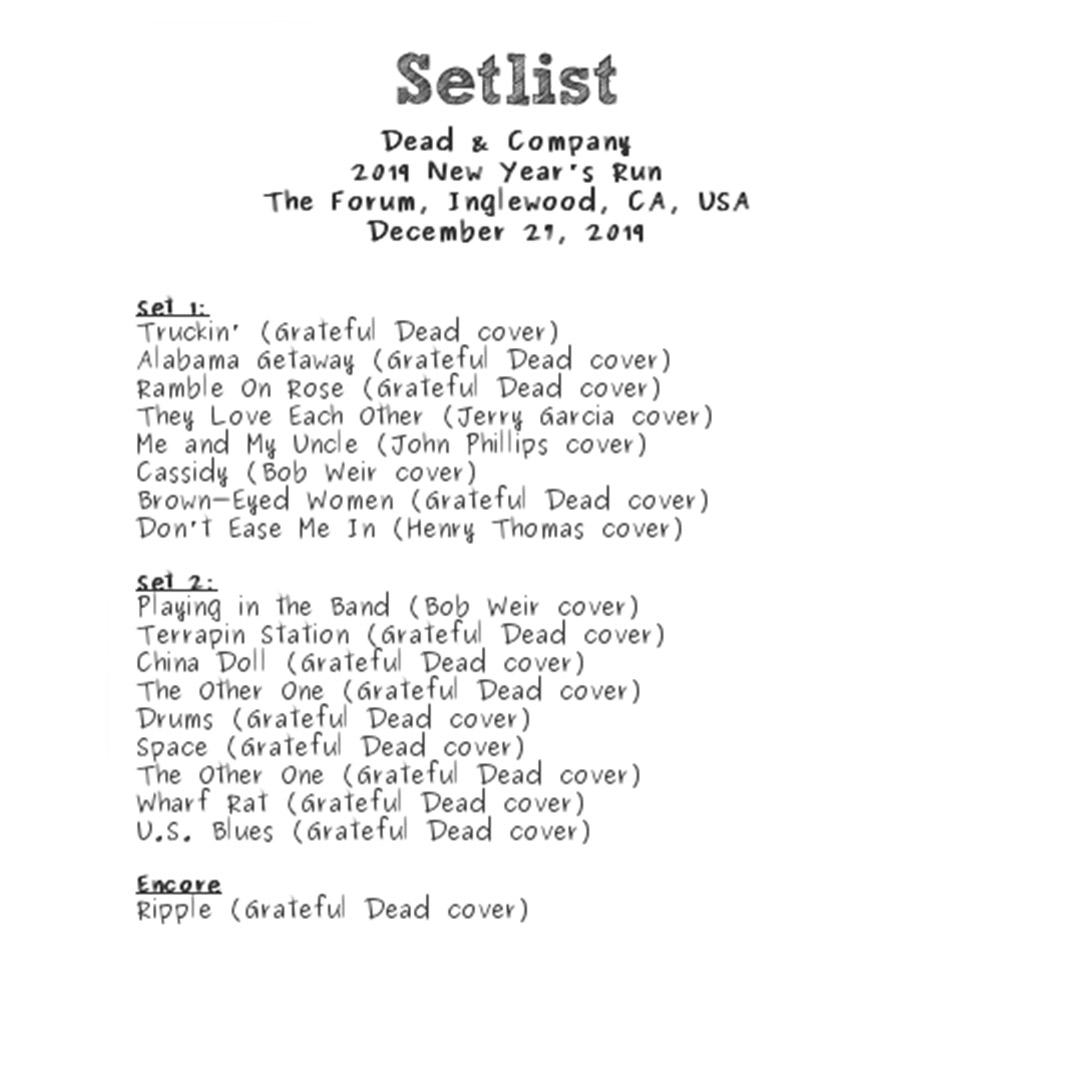
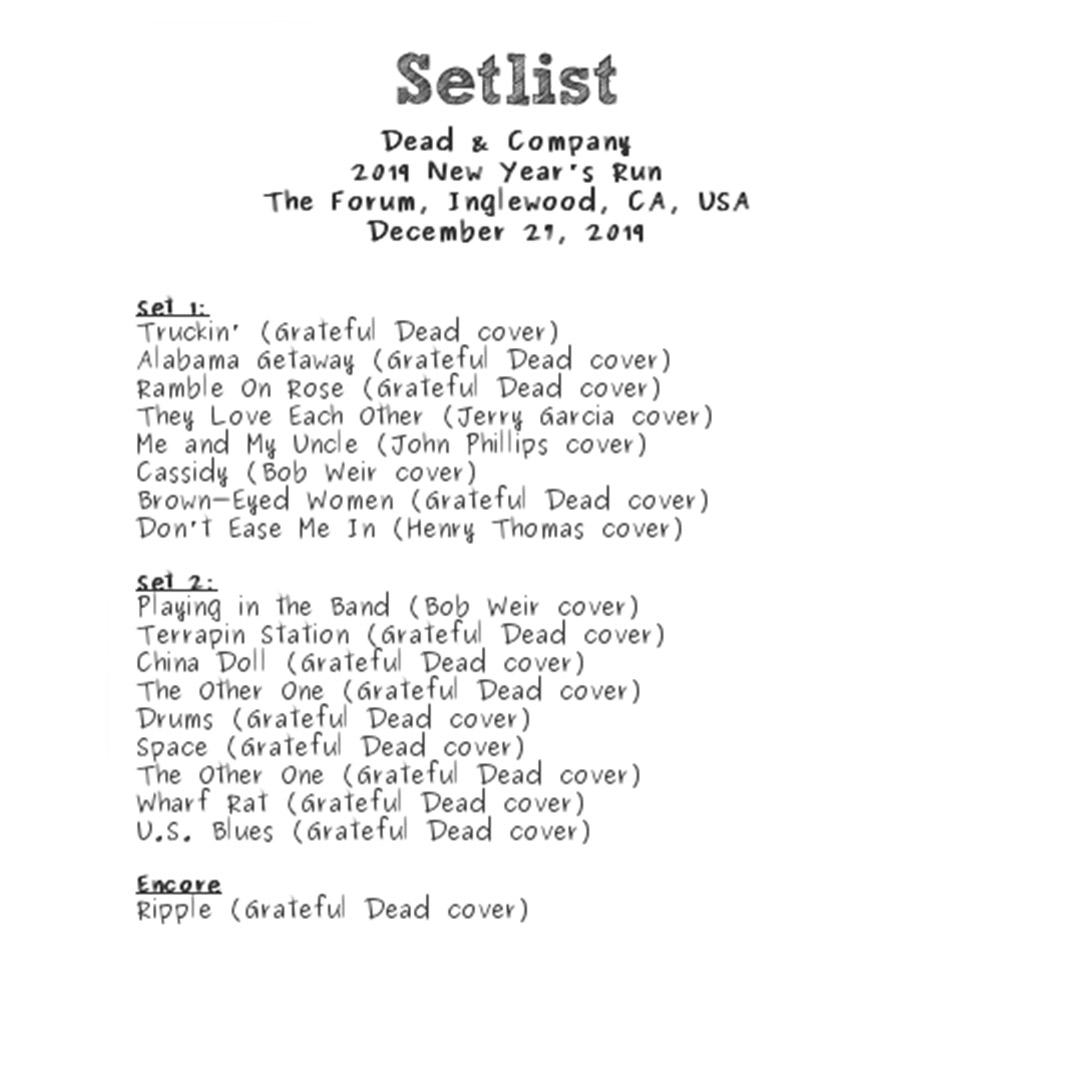
Business1 year agoDead And Co Setlist What They Played At The Gorge Amphitheatre